Who, what & why?
 In an earlier blog post Measurement of HRV we described how heart rate variability (HRV) measurements were originally performed using the Electro Cardiograph (ECG or EKG) and then later by Polar chest straps once those had been validated for beat to beat accuracy in the 1990s.
In an earlier blog post Measurement of HRV we described how heart rate variability (HRV) measurements were originally performed using the Electro Cardiograph (ECG or EKG) and then later by Polar chest straps once those had been validated for beat to beat accuracy in the 1990s.
The ithlete Finger Sensor uses the principle of photoplethysmography (PPG), which is a fancy term for measuring how blood pulses through the body’s arteries by shining light (usually infrared) through it. The Finger Sensor is closely modeled on the medical monitoring version used in all hospitals, but with the processing performed in your phone instead of a bedside monitor.
The Finger Sensor has been used in several research studies, and was validated originally by Dr James Heathers for use in a community health study in East Africa. Now, sports scientists Dr Mike Esco and Andrew Flatt have taken an in-depth look at the accuracy of the Finger Sensor in an athletic population.
What did they do?
They recruited 30 college age men and women all of whom were active, and some US national standard collegiate athletes.
All participants wore a medical ECG (Biopac MP100) as well as the ithlete Finger Sensor. At least one minute was allowed for heart rate stabilization before the ithlete app measurement was performed. The test was repeated in the lying (supine), seated, and standing positions, since all of these are popular with HRV users for different reasons. The comparison was made using the ithlete (20x LnRMSSD) scale with time-synchronized data from the Biopac ECG.
What did they find?
They found very good agreement between the mean values of HRV in all three positions:

All positions had correlations of 0.98 or higher to the gold standard ECG.
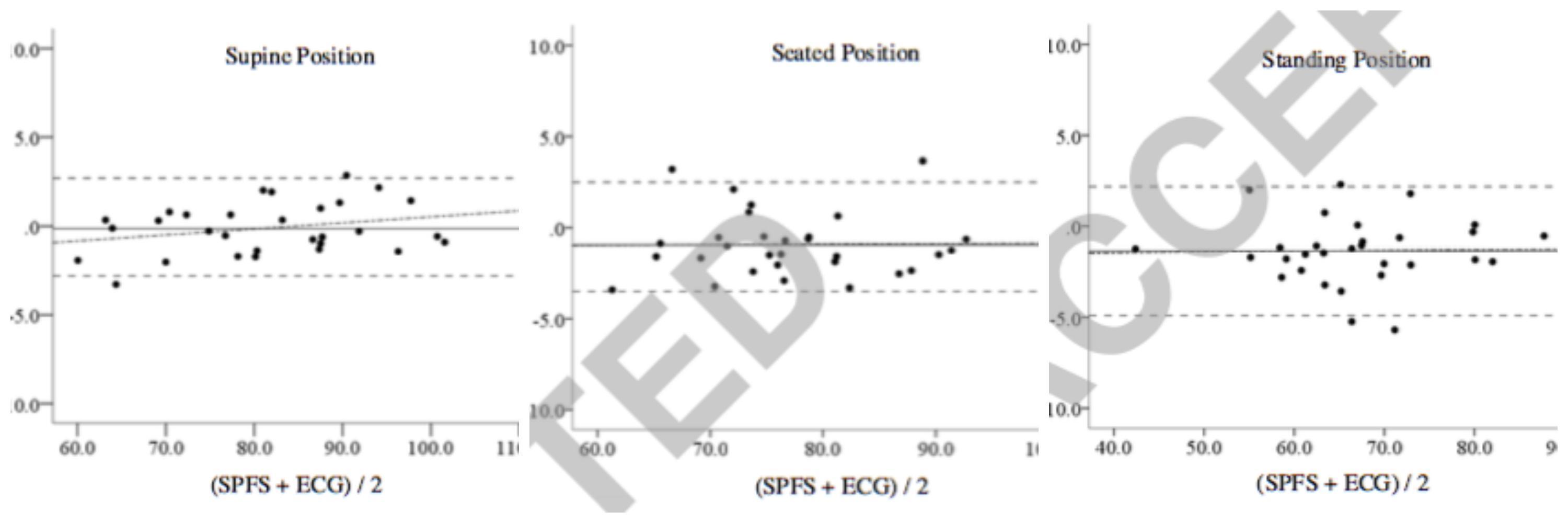
Bland-Altman plots are a standard way of revealing random and systematic differences (such as proportional biases) between two different methods, and these are shown below for the three positions:
What does it mean?
What we are looking for is low bias and tight limits of agreement, as this means we can rely on the Finger Sensor measure being a reliable substitute for the gold standard ECG, and ideally one that can be used interchangeably.
The Standard Error of Estimate averages <1.7 over all three positions, so in practical terms if you take a large number of simultaneous HRV readings you can expect there to be up to a 1.7 difference between the Finger Sensor and chest strap two thirds of the time.
When compared to the Fitbit HR accuracy study, this is significantly better, since the Fitbit devices could only manage a Standard Error of Estimate of 17 bpm for heart rate (HR), a much less demanding measure than HRV http://www.myithlete.com/blog-how-accurate-are-consumer-pulse-sensors-part-2-the-fitbit-case/
Why measure in 3 positions?
Its worth also mentioning why the Authors chose three different positions for the comparisons. In their words
“While the supine position is well tolerated in athletes, it does not promote the most appropriate position for morning measures since the subject may be at-risk of falling back to sleep. In addition, extremely low heart rates with concurrent low HRV has been noted as parasympathetic saturation of the sinoatrial node may be present when an elite aerobically trained athlete assumes a supine position. On the other hand, seated and standing positions may be more sensitive for tracking changes in autonomic activity in response to training in elite athletes.
Overall, we recommend the seated position when using the finger sensor, as it is comfortable, and you can rest your hand on a firm surface to ensure the minimum of motion disturbances (to which PPG technology is sensitive).

1 This study seems to close the debate.
2 Kudos to you Simon W for investing so much energy in this kind of sensor which few people regarded as reliable in HRV measurements which makes you a pioneer…again!
3 In photophotoplethysmography (PPG), plethysmo means augmentation.
This greek word seems used only in health investigations ( mainly for lungs ) and restricted to the meaning ” volume augmentation”
So…the question is :
– What augmentation is measured…?
( If you feel ready to give a short answer, that is )
Thanks anyway
Yves-Marie
Thank you Yves-Marie!
I understood ‘plethysmography’ to be the volumetric measurement of an organ. In this case (photoplethysmography), infrared light is shone into the finger and the amount of light transmitted is (inversely) proportional to the volume of blood in the capillaries.
Simon I recently changed from a Polar chest strap to a wrist monitor. (Mio also used by Tomtom) The chest strap has never quite worked for me, probably because I have a very bony chest , often giving a reading of 200+ during training. I have found the wrist HRM much more consistent. What I need to know is how would this influence my HRV if at all. As it happens I went down with flu symptoms at about the time I changed so I’m a bit concerned about my low HRV since then. Not sure if it is the hardware or my condition.
Hi Sonja
Although the Mio is a good tool for HR during training, its not intended to be used for HRV. That’s because it doesn’t work by measuring beat to beat intervals and includes averaging / smoothing techniques which will lower your HRV very significantly. Researcher Marco Altini explored the performance of the Mio Alpha in a blog article and concluded that it under reported by ~50%. I would continue using the chest strap for HRV – you can also put it on your back for better skin contact, or get an ithlete Finger Sensor if you have a compatible phone.
Simon that is exactly what I have found. I am so sorry that you no longer have representation in South Africa. I have been using iThlete for many years, since it arrived here, and cannot do without it particularly as I am so prone to overtraining. I’ll order a finger sensor from the UK. My piece on recovery training that I agreed to write for you will have to wait a little longer as my data is now obviously corrupt. Many, many thanks for always being there.
Hi Sonja
No worries, and thanks for all your support over the past few years!
That is exactly what I found. I am so sorry you don’t have representation in South Africa anymore. I’ll get a finger sensor from the UK. I think it’s my ECG receiver that is faulty. Have had it since you first came to SA. Can’t do without my iThlete now specially as I’m inclined to overtrain. I will need more time to write the piece on recovery training with iThlete as my data is now corrupted. Thanks Simon for always being there.
I had problems with HR belt measurements on Android so I turned to the optical sensor +IPhone . After giving it a try I would say that the “miracle” solution isn’t there. In fact, I found the HR belt to be quicker, more secure, to begin to start a measure and that resetting Android when it failed worked fine.
I keep wondering if an earlobe sensor wouldn’t be more reliable and reassuring than a finger one, even if I recognize that all the oximeters I see are finger-based.
Keep on working on such a useful/promising technique