Chronic inflammation is a major health issue and many of us will eventually succumb to an inflammatory disease. Inflammation is connected to weight gain, obesity, accelerated aging, cardiovascular disease, diabetes, asthma, arthritis, cancer, septic and digestive problems. Inflammation can shorten your life and cause you pain on a persistent daily basis.
In the case of injuries or sickness such as a sore throat, inflammation is a natural, necessary response of the immune system and is a part of healing. The long term, chronic inflammation is the kind that you need to reduce.
Several times during my researches on heart rate variability (HRV) to develop ithlete, I had seen references to possible connections between inflammation and HRV, but I had not spent sufficient time to investigate the subject properly. Recently, however I came across a review paper in the International Journal of Internal Medicine by JM Huston & KJ Tracey that explores the mechanisms by which inflammation is controlled in the body, and how both normal and stimulated levels of HRV might affect this.
The principle molecules responsible for inflammatory reaction are called cytokines, and they transmit pro-inflammatory and immuno-regulatory messages to cells throughout the body. High levels of circulating cytokines are responsible for chronic disease conditions mentioned above.
During the 1990s, the authors of this review discovered a neural control circuit that acted to keep the body’s cytokine production, and therefore inflammatory response, in check. The diagram below shows how this works, and it begins with our favourite nerve, the vagus – the same nerve that creates HRV by varying the rate at which heart beats occur!
Fig 1 – the cholinergic anti-inflammatory pathway
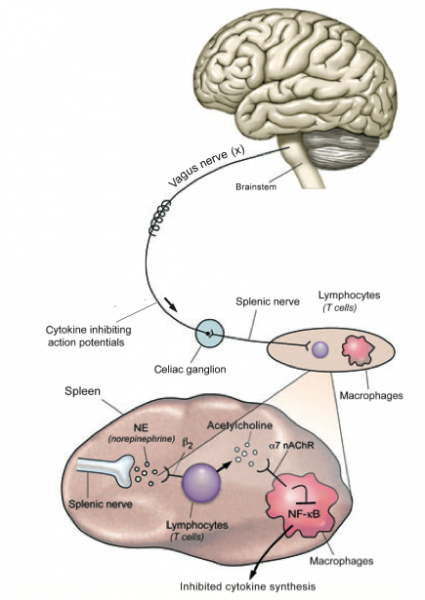
The way that this works is that signals from the brain stem travel to the spleen (which is responsible for a lot of immune system regulation) and act on particular white blood cells (lymphocytes, or T cells). These white blood cells produce nerve transmitter acetycholine to reduce the production of cytokines by macrophages in the immune system.
It’s very important to note that without the influence of the vagus nerve, cytokines are produced in much larger quantities in response to e.g. bacterial infections. The authors have demonstrated that artificially stimulating the vagus nerve controls the activation of circulating immune cells as well as production of cytokines.
As a brief, but relevant aside, some sports scientists have proposed that excessive cytokine production may be responsible for the symptoms of overtraining.
Before this mechanism was discovered, it was thought that reduced HRV in many auto immune, disease and septic conditions resulted from damage to the nerves of the parasympathetic nervous system (although this is also true in the case of Type 2 diabetes). As well as physical conditions, it is known that depression is also associated with increased cytokine production and reduced immune function, as well as reduced HRV which correlates with the severity of the depression.
Cardiovascular disease, the Western World’s biggest killer results from atherosclerosis, itself triggered by the action of cytokine produced C-reactive protein (CRP). Several studies have shown an inverse relationship between HRV and CRP levels, and also to physical activity levels, where the most physically active people demonstrate the lowest CRP, and highest HRV. It’s even proposed that the main health improving benefit of exercise is directly due to the combination of increased HRV and reduced inflammation!
The authors conclude by envisaging a future where daily or even more frequent HRV monitoring conveys important information on the condition of patients with auto-immune and long term inflammatory diseases.
For me, this paper was a real eye-opener, and increases my conviction even further to understand and make use of this knowledge in creating ithlete HRV based tools for both healthy & sick people.

Well ..They made better food choices …which i used to notice i did any time i started doing yoga
A big news story in the UK today is reported by Sky News which is based on exactly the principles of this research summary, ie artificially stimulating the vagus nerve to reduce excessive inflammatory response in the spleen. The implant technique is expected to have beneficial effects (and very few side effects) on a range of inflammatory disorders, as forecast in this research. Exciting times!
Hi Simon here’s a study that shows that chronic vagus stimulation reduced weight of mini pigs
http://www.ncbi.nlm.nih.gov/pubmed/20600417
Thanks Leo – hadn’t seen that one, and yet another reason to make exercise & lifestyle choices that chronically boost our HRV. The image of mini-pigs choosing fresh fruit salad over the icecream sundae is going to be with me for a while though…
Simon, I have recently been able to significantly raise HRV and heart coherence during chanting meditation sessions of half hour to one hour. Are you aware of any research that suggests any health benefits from temporarily raising HRV on a regular basis? I know heart math claim that temporarily maintaining coherence is ver y beneficial. I was wondering if raising HRV is as useful?
Hi Nigel,
This is an area where more solid research is needed in my view!
I’ve certainly asked myself the same question, and come to the conclusion that any period of suppression of the sympathetic nervous system that seems to be constantly activated in modern life is of benefit. The good thing about coherent breathing, for reasons which are not fully understood yet, is that it not only temporarily increases parasympathetic HRV, but also causes a longer term resetting of the baroreflex set point achieving a lasting reduction in blood pressure that could be very beneficial indeed.
You may already have listened to it, but there is a very good interview with Dr Richard Gevirtz in this episode of thequantifiedbody podcast that explores HRV biofeedback clearly & thoroughly
https://thequantifiedbody.net/heart-rate-variability-biofeedback-richard-gevirtz/
Hope this helps,
Simon.
Simon, I was recently diagnosed with paroxysmal atrial fibrillation. I have only experienced 6 episodes and they have all occurred during periods of extreme physical activity (hr>140 Bpm). Only with the most recent one have I required a cardioversion. My resting heart rate is 48 Bpm and I typically ride a bicycle 4-5 hours/week. Has there been any research regarding use of HRV to avoid atrial fibrillation episodes?
Hi Dave,
Sorry to hear you are suffering from AF. I have a number of friends with Af brought on by years of endurance training, and have looked at whether HRV can be used to predict an episode. Unfortunately, neither the research, nor experiments we did have discovered anything very concrete. The most help has been lifestyle diaries including details of food & stress levels, though of course the ithlete subjective sliders & comments can help in recording this. Nearly all those I know have cut out caffeine and found it helps. Do please let us know if you find any reliable trends or predictions.